PICC Line Occlusions: Understanding the How and Why for Prevention
By Nancy Moureau, PhD, RN, CRNI, CPUI, VA-BC
According to iData Research (iData Research, Vascular Access Devices Market Analysis, 2020-2026 MedSuite, Vancouver, BC), more than 340 million peripheral (PIV) and 7 million central venous catheters (CVC) are purchased for use each year in the USA.1 More than 30% of patients with vascular access devices (VAD) will experience complications. Millions of catheter complications occur annually, including catheter failure or removal from occlusion, catheter-related thrombosis, or catheter-associated bloodstream infections. Maintaining the function and patency of these VADs is necessary to effectively administer intravenous medication treatments, avoid costly replacement or thrombolytic treatment, and safeguard patients from more serious infectious complications. The most common complication impacting patency and function for VADs is catheter occlusion, with an estimated incidence of 14-38%.2,3,4
We know that blood and cellular deposits on the surface of catheters develop within minutes of insertion, promoting fibrin formation, lumen occlusion, and potentially trapping bacteria in this conditioning layer. When the foreign substance of catheter material is inserted into the bloodstream, a conditioning layer is formed and absorbed onto the catheter surface, triggering a complex series of biological responses including protein absorption, platelet adhesion, and thrombosis.5 Cellular deposits that build up on the inner and outer surfaces of catheters cause catheter dysfunction, partial or total occlusion, and inability to flush or infuse, often requiring catheter replacement.
Since cellular adhesion and occlusion are so common, given new technologies and clinical practices, why do these problems persist? Catheter occlusion is multifactorial including device, patient, and clinician factors.6 As described, the material used for VADs, different formulations of polyurethane and silicone, are recognized as foreign substances promoting a body response that attempts to engulf and eliminate the VAD. Depending on the patient's comorbidities, clotting factors, medications, and other risk factors, hypercoagulation may be a component of occlusion for that patient. Working against the normal body response to foreign materials and thrombotic risk factors of the patient, clinicians perform catheter flushing and clamping sequences to maintain patency. A clear understanding of these factors is necessary for the clinician to maintain catheter function and avoid complications.
To prevent occlusion and VAD complications, special attention is needed for the education of clinicians, integration of the best functioning add-on devices, and the best catheter materials.7,8 Staff understanding of the management of VADs with good disinfection prior to connection, assessment of function, regular pulsatile flushing, and even the function of devices like needleless connectors, all work together toward ensuring the patient has trouble-free intravenous treatments. Consideration should be given to using valved needleless connectors, catheters, and tubing to promote the maintenance of catheter patency. Anti-reflux, needleless connectors include an integrated valve that prevents blood movement into a catheter, reducing the exposure of the catheter to what could be layer upon layer of blood cells with each muscle movement, connection, or disconnection for infusions.9,10 New catheter materials should be evaluated to identify those with the lowest incidence of cell adhesion.11,12,13
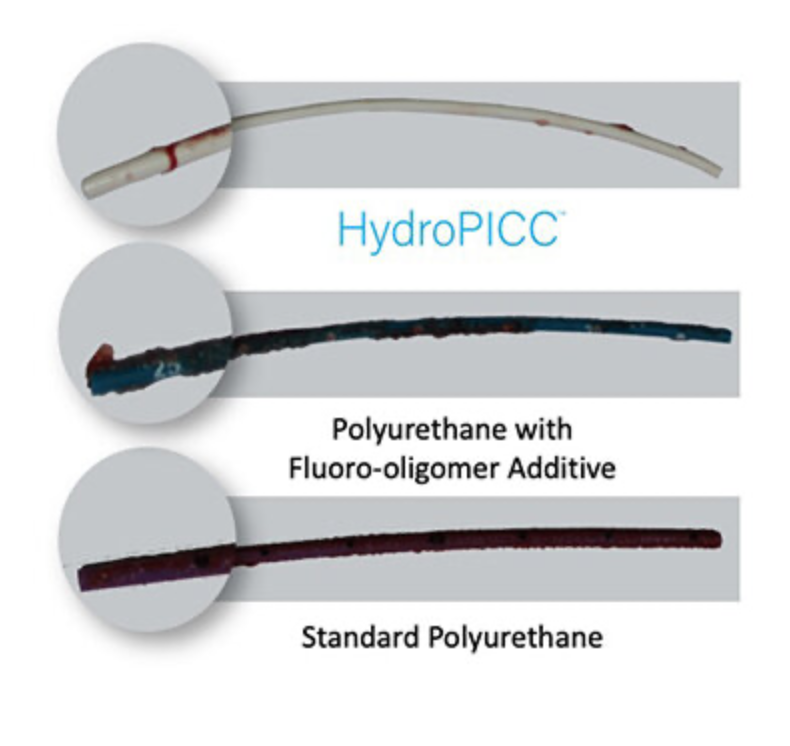
Catheter coatings and impregnations have a positive effect of reducing infection colonization and thrombosis in the short term. Material composition changes that result in longer-term surface lubrication show the most significant promise for reducing the foreign body response, cellular adhesion, and occlusion complications.
Blood coagulation with platelet adhesion to intraluminal catheter surfaces remains one of the most significant contributors to vascular access catheter dysfunction by producing partial and total VAD catheter occlusion.4 Preventing thrombosis, catheter occlusion, and infection are high priorities for maintaining catheter function for infusions. New catheter materials may provide a method for preventing these common complications with PICC and Midline catheters. These catheter materials may herald a new age of improved patient outcomes and cost savings for healthcare facilities.
References
iData Research, Vascular Access Devices Market Analysis, Global 2020-202,6 MedSuite, iData Research, Vancouver, British Columbia, Canada.
Baskin JL, Pui CH, Reiss U, Wilimas JA, Metzger ML, Ribeiro RC, Howard SC. Management of occlusion and thrombosis associated with long-term indwelling central venous catheters. The Lancet. 2009 Jul 11;374(9684):159-69.
Hawthorn A, Bulmer AC, Mosawy S, Keogh S. Implications for maintaining vascular access device patency and performance: Application of science to practice. The journal of vascular access. 2019 Sep;20(5):461-70.
Moureau N, Poole S, Murdock MA, Gray SM, Semba CP. Central venous catheters in home infusion care: outcomes analysis in 50,470 patients. Journal of Vascular and Interventional Radiology. 2002 Oct 1;13(10):1009-16.
Moureau N. Reducing Catheter Occlusions and Failure. Healthcare Hygiene Magazine. February 2021. Accessed Dec 2022 https://viewer.joomag.com/healthcare-hygiene-magazine-february-2021-february-2021/0337892001612825262?page=44
Keogh S, Hawthorn AM, Shibeeb S, Gurney L, Pennell EN, Sabapathy S, Rickard CM, Bulmer AC. Impact of Different Flushing Frequencies on Peripheral Intravenous Catheter Failure, Coagulation, and Tissue Injury—A Counterbalanced Preclinical Human Trial. Journal of the Association for Vascular Access (2022) 27 (2): 19–29. https://doi.org/10.2309/JAVA-D-22-00006
Moureau NL. Vessel health and preservation: the right approach for vascular access. Springer Nature; 2019.
Moureau NL, Carr PJ. Vessel Health and Preservation: a model and clinical pathway for using vascular access devices. British Journal of Nursing. 2018 Apr 26;27(8):S28-35.
Hull GJ, Moureau NL, Sengupta S. Quantitative assessment of reflux in commercially available needle-free IV connectors. J Vasc Access. 2018;19(1);12-22. doi:10.5301/jva.5000781
Jasinsky L, Wurster J. Occlusion reduction and heparin elimination trial using an antireflux device on peripheral and central venous catheters. J Infus Nurs. 2009;32(1):33-39. doi:10.1097/NAN.0b013e3181921c56
Aswathy SH, Narendrakumar U, Manjubala I. Commercial hydrogels for biomedical applications. Heliyon. 2020 Apr 1;6(4):e03719.
A retrospective assessment of peripheral midline failures focusing on catheter composition. J Infus Nurs. 2022;45(5):1-9. DOI: 10.1097/NAN.0000000000000484
Mannarino MM, Bassett M, Donahue DT, Biggins JF. Novel high-strength thromboresistant poly (vinyl alcohol)-based hydrogel for vascular access applications. Journal of Biomaterials Science, Polymer Edition. 2020 Mar 23;31(5):601-21.ww