The Implication of Complications
By Eddie Korycka, MSN, RN
Complications from vascular access devices can prove deadly to patients and detrimental to hospital economics with reimbursement penalties tied to these complications. The good news is they can be greatly reduced with targeted tracking and common-sense measures.
I’ve seen the entire range of complications - from nuisance to life threatening - but nearly all are avoidable. By understanding the different types of complications and why they happen, health systems can help prevent future instances and improve outcomes for both patients and clinicians. In this post, I’ll look at two common complications and how systems could reduce their occurrence.
Even the most basic complication can delay therapy and have real time and cost implications for patients and health systems. By carefully evaluating these occurrences, systems can help better gauge the quality of a vascular access program and prevent future issues.
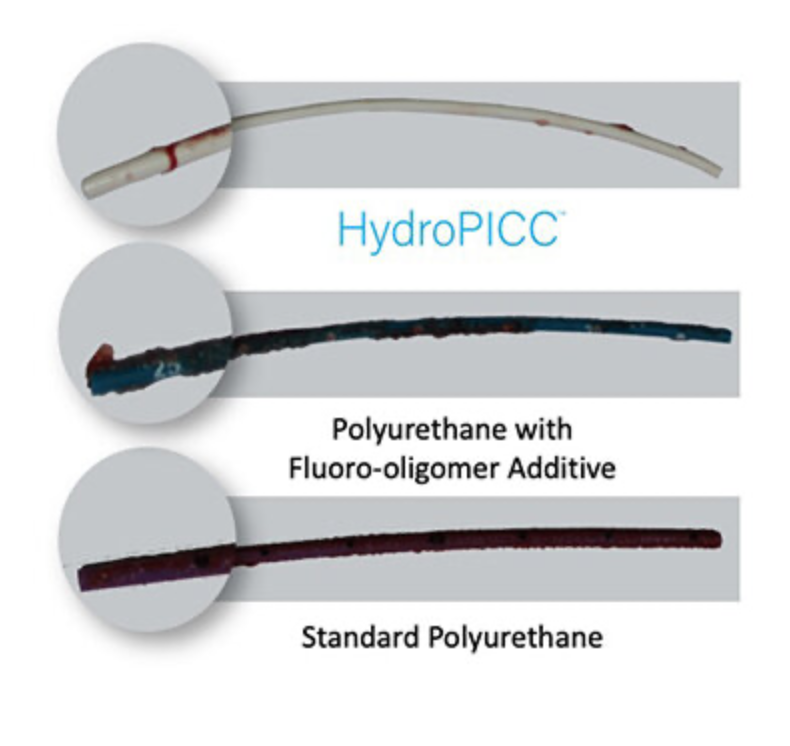
For example, phlebitis presents in as many as 63% of patients with vascular access. It can be caused by a mechanical, bacterial, or chemical issue, and could negatively impact dwell time.
By correlating the occurrences of phlebitis with the device being used, what is being infused, the antiseptic technique being utilized and the securement practice, health systems can better identify the most recurring causes of phlebitis to reduce its prevalence and improve overall dwell time.
With rates of up to 34%, infiltration is another leading vascular access complication. It happens when an infusate is unintentionally infused into the tissues external to the vessel. At first blush this might seem like a minor nuisance, but it can lead to extravasation (tissue damage caused by the infused medication) and become catastrophic for the patient.
The key to remedying this complication is the popular real estate mantra “location, location, location”. This is because the most prominent veins are often in the worst location. Peripheral IVs placed on the hand or near joints are subject to more motion, which can cause mechanical phlebitis or migrate the catheter out of the vein.
Systems could analyze infiltration rates against the location of the catheter to identify the worst offenders. Clinicians can also use ultrasound to place catheters in more ideal locations and ensure that two thirds of a placed catheter is within the vein (to avoid dislodgement).
Assessing patients for signs of vascular complications is always a critical aspect of a clinician’s job. But systems can make an added investment in quality by analyzing trends in these complications over time and against relevant criteria. By sharing these observations and improvements broadly, we can help our patients – protect our reimbursement – and ultimately improve vascular access for everyone
I would love to hear how measuring complications has improved your program in the comments section below. And I will explore more complications and potential solutions in a future post.